

In this post, Amy Clair and Emma Baker, from the University of Adelaide, discuss their research on the impact of cold homes on people’s mental health.
Why did we do this?
There is a wealth of robust evidence confirming that cold homes negatively impact people’s health. The World Health Organization recommends that temperatures of at least 21°C in living rooms and 18°C in bedrooms provides a healthy living environment.
For people living in cold homes, the most widely documented health effects tend to be physical – for example respiratory disorders or cardiovascular disease, but recent work has highlighted the importance of harder to measure mental health effects. People who live in homes that they are unable to keep suitably warm report reduced feelings of autonomy and control, impacts on sleep, reduced social activities, as well as financial strain. These pathways all potentially contribute towards poorer mental health.
What data did we use?
We used data from Understanding Society (the UK Household Longitudinal Study) that covered 2009 (when its first wave was conducted) to 2021 (wave 11, the most recent data collection). Understanding Society has a number of advantages for this type of research. Firstly its longitudinal nature allows us to track people’s housing experiences alongside their mental health, over time. Secondly, the dataset includes well established and validated measures of mental health (we used the General Health Questionnaire) as well as questions detailing perceptions of indoor temperature, alongside information on other important aspects of people’s lives, such as their employment, demographics, and financial situation.
To ensure that we were studying the impact of housing on health, and not vice versa, we restricted our analysis to those that were living in suitably warm homes on entry to the survey. We further limited our analysis to people that 1) showed no mental distress on entry to the survey, and 2) had borderline levels of mental distress on entry to the survey. For our outcome, we focused on the GHQ’s classification of ‘severe mental distress’. The large sample size provided by Understanding Society means that we were able to apply these restrictions yet still have sufficient samples to conduct multilevel discrete-time event analysis, and control for elements of their broader lives.
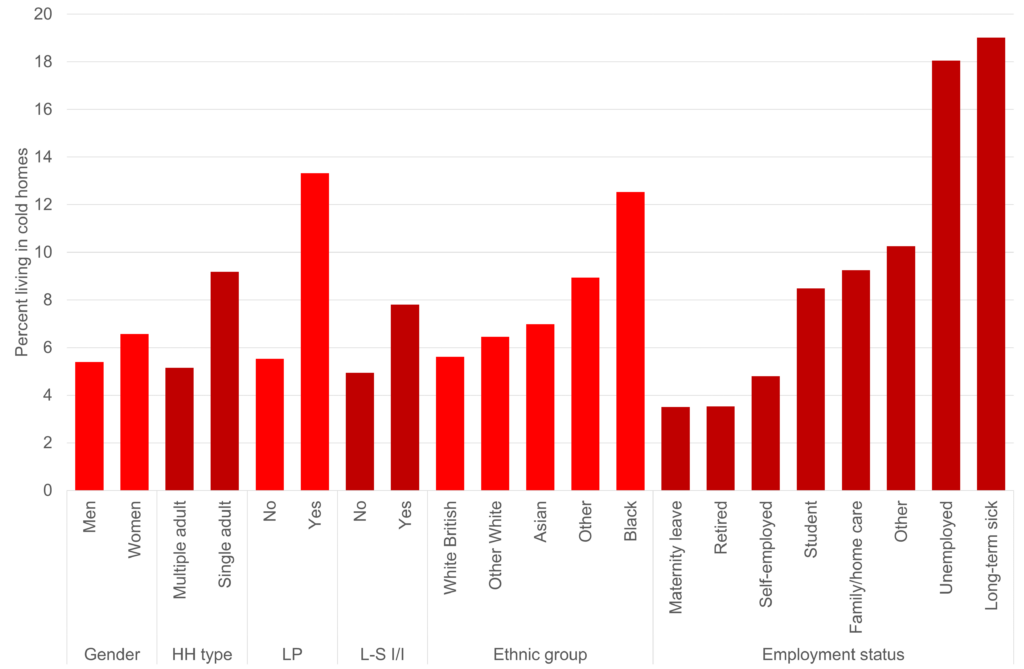
Chart 1: Percent living in cold homes, demographics. Note: HH type = household type; LP = Lone parent in household; L-S I/I = longstanding illness or impairment.
What did we find?
Firstly, the risk of living in a cold home was very unevenly distributed. Lone parents, those with a longstanding illness, the unemployed and economically inactive due to illness were all disproportionately likely to live in cold homes. Broadly, and concerningly, this suggests that the UKs sickest and most vulnerable tend to live in the housing most likely to make them sick. There were also significant inequalities across ethnic groups – 12% of Black respondents reported living in cold homes, more than double the percentage of White British respondents (5.6%). There were also significant differences across housing tenures and building types – renters were much more likely to report being cold (3% of owners reported being cold compared to 13% of social renters and 11% of private renters) for example.
In terms of the impact of becoming cold on mental health the analysis showed that, even after controlling for a range of important factors including employment and income, becoming unable to keep the home adequately warm is associated with statistically significant increases in the odds of reporting severe mental distress. For people who showed no mental distress on entry to the survey their odds of reporting severe mental distress doubled if their home became too cold. For those who had borderline mental distress their odds tripled. Keeping homes suitably warm is therefore important for mental, as well as physical, health.
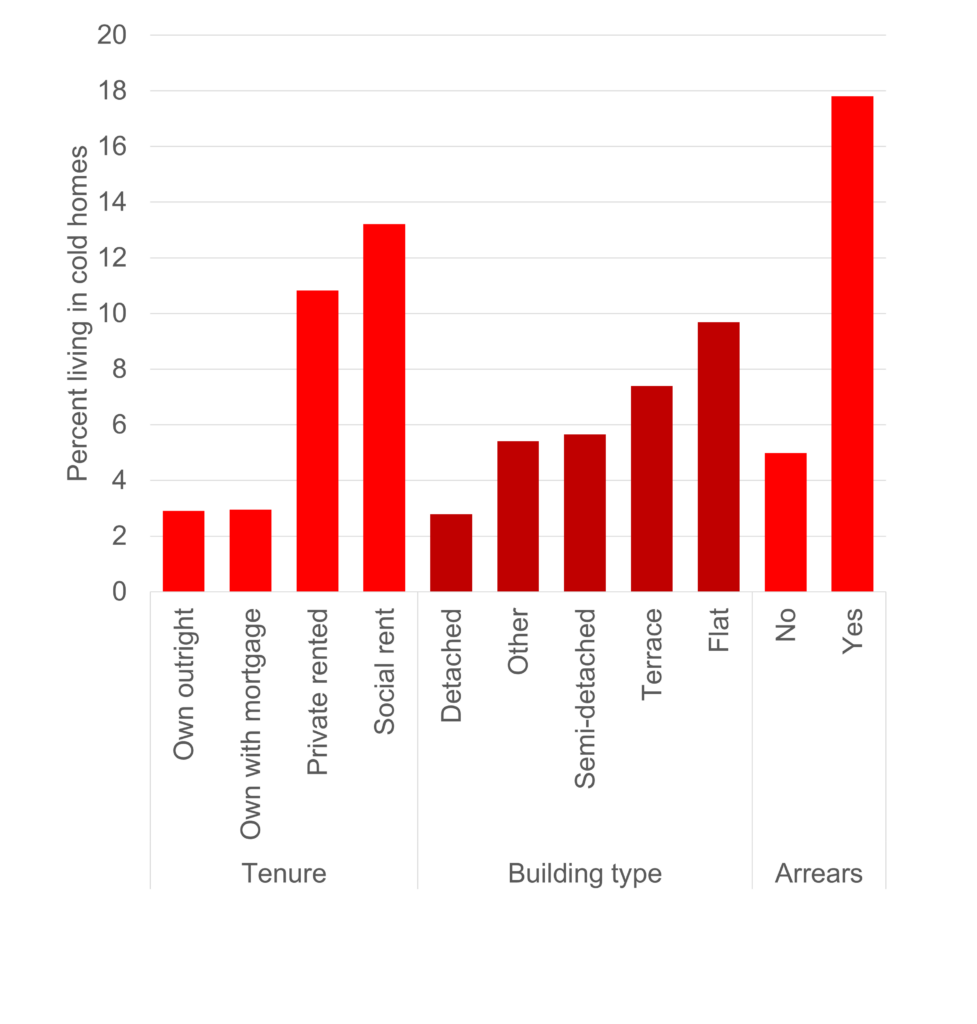
Chart 2: Percent living in cold homes, housing variables. Note: Arrears = housing payment arrears.
What are the implications?
Our analysis highlights the detrimental effect of cold housing on mental health, with a striking scale of effect, especially for people who are already at the edges of severe mental health problems. The analysis also reveals the unevenness across the population of vulnerability to having cold housing, and the worrying fact that people with other forms of disadvantage, illness and disability are most likely to have housing that is cold. This is particularly relevant at a time of high energy costs and increased financial difficulty. Cold homes are an easy target for policy intervention, and our results support calls for improved energy efficiency in homes and greater financial support for those struggling. Reducing the number of people living in homes that they are unable to keep suitably warm, whether due to energy inefficiency or financial constraints, has the potential to reduce mental health problems, health inequalities, and health spending, with potential positive consequences for employment and productivity.
Next steps
Our analysis focuses on adults only. An important next step will be to explore the impact of cold homes on the mental health of children. It is likely that children, particularly older children, experience many of the same impacts as adults, however it is important to study children in their own right.
The research presented in this blog post is based on Amy and Emma’s recent publication which can be viewed online.
About the authors
Amy Clair is a researcher in the Australian Centre for Housing Research, University of Adelaide, and research associate of the ESRC Centre on Micro-Social Change, University of Essex. A quantitative social policy researcher, her work focuses on the impact of policy on health and well-being, with an emphasis on housing and child well-being. Recent work has explored the impact of cold homes on mental health, changes to the Local Housing Allowance, and the implications of the COVID-19 pandemic for social policy.
Emma Baker is Professor of Housing Research at the University of Adelaide and Deputy Director of the NHMRC Centre for Research Excellence in Healthy Housing. Her work examines the health and human impacts of housing and location in urban and regional environments, producing academic, as well as policy-relevant research. Driving this work is a conceptual focus on housing and location as a social determinant of health and an interest in analyses that utilise longitudinal, spatial and administrative big data. Recent academic and policy publications include commissioned policy background papers for the planning and housing strategies of South Australia, the construction of the third in a series of publicly accessible national housing conditions datasets, an analysis of the effects of cold housing on individual health, and papers analysing the influence of multiple housing problems on health and wellbeing.
This blog post contributes to our ongoing work looking at Housing and homelessness in data and Mental health in data.
