

Dr Natasha Chilman and Dr Sarah Markham describe a new study looking at mental health and multimorbidity for people with prior experiences of homelessness in a household survey.
Homelessness is an increasing societal and public health emergency, particularly in the United Kingdom – we have the highest rate of homelessness compared to other high-income countries.
Most of the research in this area has focused on people who are currently experiencing homelessness, but for many people homelessness is a temporary and impactful experience in their lifetime. This begs the question – do we see health inequalities for people who have formerly experienced homelessness longer-term, after moving into rented or owned accommodation?
To better understand this, Natasha and colleagues analysed data from the Adult Psychiatric Morbidity Surveys. This is a nationally representative dataset of people living in private households. Associations between experiences of former homelessness and health were investigated, including anxiety, depression, physical health conditions, alcohol and substance dependence, and multimorbidity (co-occurring health conditions).
Sarah worked with Natasha to advise on the study from the early stages, together with eight people with lived experience of homelessness who were connected to the charities Rethink Mental Illness and Pathway. This had several benefits for the research process. For example, as someone with lived experience of homelessness and help seeking, Sarah found she was able to bring synergy to the research process via experiential learning to help bring the data alive.
In the total complete survey sample of 13,859 participants, 535 people reported a previous experience of homelessness, the majority of whom last experienced homelessness in adulthood over 6-months before the surveys (82%). The key findings from the analyses were:
- Almost half (45%) of people who formerly experienced homelessness were currently experiencing depression and/or anxiety, compared to 15% of people who had never experienced homelessness. Symptoms of these mental health conditions were also more severe for people who formerly experienced homelessness.
- Former homelessness was strongly associated with mental health conditions, physical health conditions, alcohol and substance dependence problems, and multimorbidities (conditions in combination), even after adjusting for demographic characteristics, indicators of socio-economic position and smoking in models.
- Population attributable fractions, which estimate the proportion of the health outcome attributable to former homelessness, were disproportionately high for alcohol and substance dependence in the private household population.
- People who formerly experienced homelessness were more likely to experience other life course adversities such as bullying and violence. When adjusting for these adversities in the statistical models, former homelessness was still associated with mental and physical health inequalities, but not substance or alcohol dependence inequalities.
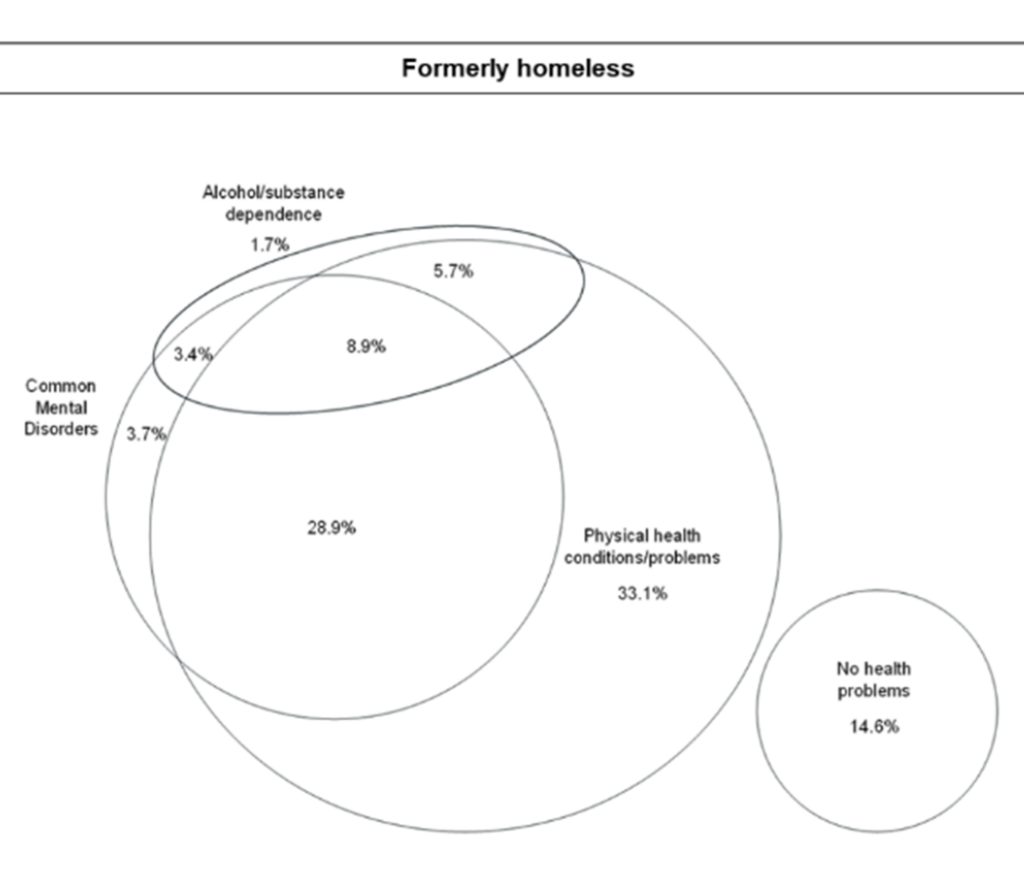
These findings paint a concerning picture, where people experience long-lasting inequalities in their health following experiences of homelessness.
When discussing this in the advisory groups with people with lived experience, it was highlighted that these results (while not necessarily surprising in the directions of associations) were shocking in scale. It was noted that this indicates that a roof over someone’s head is not enough, which was felt to resonate with the lived experience of some of the members of the involvement groups. From Sarah’s perspective, this research highlights the need to invest in all dimensions of a person’s life to support and empower them.
This research has relevance to the NICE guidelines for supporting people experiencing homelessness, as the findings illustrate the importance of long-term, integrated healthcare that extends post-homelessness and takes a trauma-informed approach.
To broadcast these findings to clinicians in England, we co-presented at a Pathway primary care event last year. Natasha also presented this research on a global stage at the World Congress of Epidemiology, which prompted discussions on the importance of the representation of people who experience homelessness in national large-scale epidemiological datasets. You can read more about the study in the paper.
Natasha can be contacted at natasha.chilman@kcl.ac.uk.
About the authors
Dr Natasha Chilman is a Teaching Fellow and Research Associate at King’s College London for the UKRI Population Health Improvement (PHI-UK) Population Mental Health Consortium. She conducted this study as part of her PhD research funded by the LISS-DTP. She was a 2023 UKDS Data Impact Fellow.
Dr Sarah Markham, who advised on the study, is a pure mathematician with lived experience of mental health conditions and homelessness. She uses her lived experience to advocate for others and advance human rights based practice and policy throughout mental health, social care and public health.
